I
assume most of you have something to do with the kidney. In my regular
life I come close to nephrologists only when I need their help to
dialyze a patient with poorly treated diabetes. I do hope that by the
end of this exercise we learn how to do a better job and reduce the
number of patients who land in the dialysis center.
|
 |
Nobody doubts anymore that there
is a diabetes pandemic in the world. In fact, Dr. King of the World
Health Organization (WHO) has projected that by the year 2025, there
will be at least 300 million persons with diabetes worldwide; that would
roughly represent a doubling of the rate from about the year 2000. So,
there is an epidemic, and the vast majority of persons who develop
diabetes will have type 2 diabetes. We also are seeing increases in the
prevalence and incidence rates of type 1 diabetes across the world, but
the magnitude of increase is nowhere near what we see with type 2.
|
 |
The overwhelming explanation for
the diabetes pandemic is attributable to type 2 diabetes; the natural
history and pathophysiology of this disease has been increasingly
understood. We now know that in persons selected by their genetic makeup
and stressed by the environment, very early changes begin to occur in
glucoregulatory physiology that translate to insulin resistance. Even in
that early stage of "dysglycemia" -- where the blood glucose numbers
are still, technically, within the normal range; and with regard to
diabetes diagnosis, they are nondiabetic -- you begin to see changes in
lipids that are unfavorable, specifically small decreases in
high-density lipoprotein (HDL), the protective cholesterol, and
increases in triglycerides. About that time, people also begin to accrue
increases in both systolic and diastolic blood pressure numbers but
they still do not qualify for diabetes diagnosis.
With insulin resistance comes a
demand for greater and greater secretion of insulin. The natural
biologic response to a resistant state is overproduction of the signal
hormonal ligand; the beta cells of the pancreas are called upon to work
harder and harder to produce more and more insulin. This
insulin-resistant hyperinsulinemic phase is really a prodromal phase for
future diabetes, a prodrome that "crosses the Rubicon" when people
begin to wake up with fasting glucose greater than 99 mg/dL. The
individual whose fasting glucose reaches 100 mg/dL is no longer
considered normal; 100 mg/dL in the fasting state now has a new name,
impaired fasting glucose (IFG), and 126 mg/dL, as you all know, is
diabetes in the fasting state.
We have people in these
prediabetic stages of IFG and impaired glucose tolerance (IGT), and they
stay there for variable periods, depending on genetic makeup and other
stressors. Some may evolve rapidly to overt type 2 diabetes, others may
not progress that rapidly, and yet some others might even recover from
this intermediate stage. We call that reversion to normal glucose
tolerance. In those who are destined to move on to diabetes, we see the
glucose numbers creep up into diagnostic ranges, and they are identified
as patients with diabetes and treated accordingly.
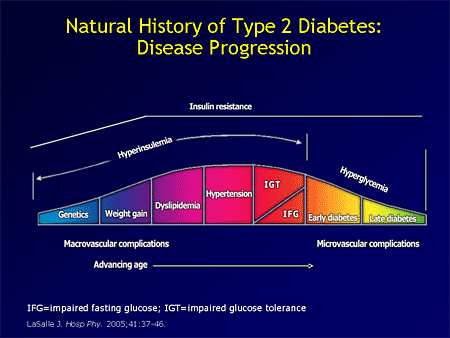
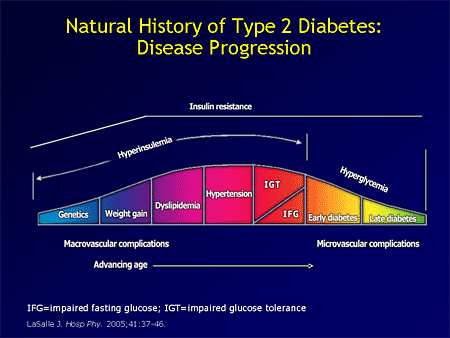
This is a conceptual slide from a
review article by LaSalle, who is a primary care physician with great
interest in diabetes and has been honing his skills in the area of
diabetes research. Notice that eye damage and kidney damage -- the type
you deal with in diabetic nephropathy, as well as diabetic neuropathy,
the so-called, "microvascular complications" -- do not begin to occur
until after the hyperglycemia has occurred. They are glucose-driven,
glucocentric complications.
However, long before the clock
starts ticking for microvascular complications, you notice the
beginnings of risk factors of macrovascular disease, such as
dyslipidemia and hypertension, which together with other
atheroinflammatory mediators, will set the stage for atherosclerosis.
So, this occurs at an earlier time point.
|
 |
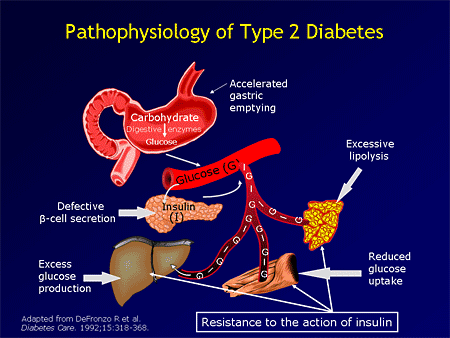
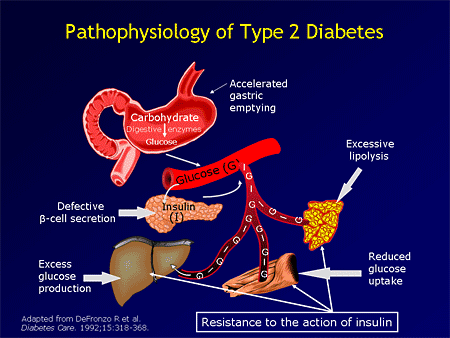
But, getting back to the diabetes
epidemic, and specifically to the pathophysiology of type 2 diabetes.
We now know that there are multiple contributors to the eventual
occurrence of hyperglycemia, chief among these is a change in tissue
response to insulin. Insulin is the ultimate anabolic hormone that has
major influences in the metabolism of glucose, protein, fatty acids,
salt and water, and even memory facilitation in the central nervous
system, among others. Yet, in persons who have inherited diabetes -- a
set of diabetogens from their blood line -- who then also are confronted
by environmental challenges, such as obesity or physical inactivity,
these risk factors collude to uncover a state that, for lack of a better
description, is called insulin resistance. That state is all-pervasive;
every cell is involved in that perturbation. The simplest construct for
understanding insulin resistance, almost a simplistic approach, is to
measure insulin-stimulated glucose uptake by the tissues. If you did
that years, and sometimes decades, before the occurrence of type 2
diabetes, individuals at risk might begin to fail that test -- the
insulin sensitivity test, where you measure impairment in
insulin-stimulated glucose transport. But, that is only one way of
identifying insulin resistance. There are many other pathways of insulin
signaling for which we, currently, do not have routine measurements or
convenient tools to probe at a clinical level.
This insulin resistance precedes
the occurrence of type 2 diabetes, but it does not go away when the
diabetes has occurred. It hangs in there and continues to negate the
effect of any treatments we bring to bear on the diabetes, unless such
treatments specifically address the resistance; and that is a very
important therapeutic point to make.
Now, in addition to insulin
resistance, the beta cells of the pancreas play a leading role in
allowing diabetes to occur. After all, you can induce all the insulin
resistance in the world in a given subject; but, if their pancreas
responds appropriately, by secreting tons and tons of insulin, the blood
glucose will stay in the normal range. So, it is the failure of the
beta cells of the pancreas to adequately compensate for progressive
insulin resistance that becomes the denouement, the ultimate straw that
breaks the proverbial camel's back and allows hyperglycemia to occur.
So, insulin resistance is necessary, but not sufficient, to cause
diabetes. A second hit, a second defect, residing within the beta cells
of the pancreas allows for the diabetes to manifest; and that defect in
the beta cell itself is now believed to be largely inherited. So, people
in diabetes families would have a set of genes that predicts the
insulin resistance and, perhaps, another set that predicts apoptosis, or
increased cell death, within the Islets of Langerhans that prevents
them from mounting a sufficiently robust insulin secretory response.
Many will not know this
intuitively, but it is true that gastric emptying rates are accelerated
in people with diabetes. When you encounter diabetes in the context of
gastroparesis, you tend to think that the bowels are sluggish in people
with diabetes; but, actually, the primary motility defect in diabetes is
accelerated gastric emptying. Some of the newer agents that have been
introduced have actually worked on diabetes by slowing down the gastric
emptying rate. Some of the incretin agents work on that.
The other defect that we are
beginning to understand in diabetes comes out of the adipocytes;
lipolytic products like glycerol, free fatty acids can be used by the
liver to produce more glucose molecules. Other adipocytokines that come
out of the fat cells also are turning out to be very bad for glucose
metabolism, by inducing insulin resistance and other processes.
Finally, the liver plays a key
role in the final pathogenesis of type 2 diabetes. Remember that the
liver is a glucose factory, producing on average 1 mg glucose/lb of body
weight/min. When people have type 2 diabetes, their average glucose
production rate increases from the normal value of 1 mg/lb/min to 2 to 3
mg/lb/min. There are 1440 minutes a day; when you do the math, you can
readily appreciate how much glucose is coming out of the liver. That
number can be doubled or tripled if you are dealing with a diabetic
patient.
Interestingly, all of these
pathophysiologic defects in type 2 diabetes also are veritable targets
for drug development. We have at least 1 drug on the market that will be
addressing each of these targets.
|
 |
Beta Cell Defects and Diabetes Outcomes
Let me spend a moment on the beta
cell defect, because it is really the Achilles' heel of type 2 diabetes
pathophysiology. If you take away somebody's pancreas, you convert them
immediately to diabetes; if you do a total pancreatectomy, if you
deprive a system of insulin, that system immediately becomes diabetic.
But, if you increase insulin resistance inordinately highly, you still
do not have 100% straightforward diabetes, as long as the beta cells of
the pancreas are rising to the challenge.
The failure of the beta cells to
rescue nearly 20 million Americans who already have developed diabetes
and 300 million people in the world who will develop diabetes by the
year 2025 is an important research matter. We are not quite sure why the
beta cells are failing. We do know that the cell mass decreases and
that the mechanism of cell mass loss is through programmed cell death,
or apoptosis. These triggers for the apoptosis, however, are not well
known, but we do have candidates. Time will not permit me to really
flesh out this slide, but suffice it to say that current research has
accorded priority to elucidation of the mechanism for beta cell death in
type 2 diabetes. Numerous targets, including immunologic targets,
lipotoxicity, and hyperglycemia itself, have been identified as a signal
for cell dysfunction.
Above certain thresholds of
ambient blood glucose levels, the beta cells begin to take a hit; we
call it glucose toxicity. They begin to be affected down to the genomic
level, where the transcription and translation of the insulin gene
becomes impaired by ambient hyperglycemia. That is a reversible cause of
beta cell dysfunction.
|
|
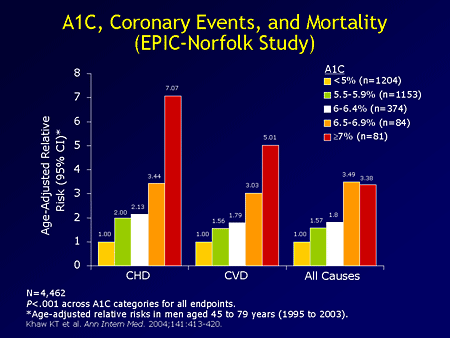
If we go back to the diabetes
epidemic, one of the most worrisome signs from the clinical research
field is that one does not need to have big scale increases in blood
glucose to begin to suffer dire consequences. There is a study coming
out of the United Kingdom called the European Prospective Investigation
Into Cancer (EPIC). It is a cancer-focused study, and in one of the
study sites, in Norfolk County in England, they had enough measurements
of biochemical values, glucose values, over several years to allow
analysis.
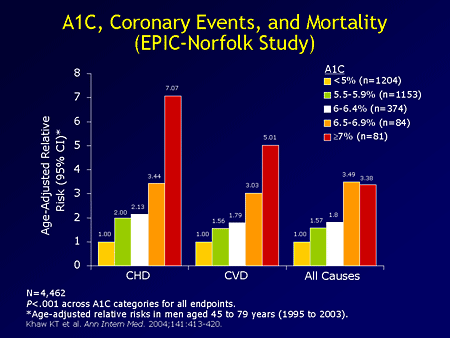
What you see on the screen is
cardiovascular mortality, outcomes data, on the basis of shifts in blood
glucose levels captured by the hemoglobin A1c within reasonably normal
ranges of life. If you look at physiologic ranges of hemoglobin A1c,
people without diabetes score from about 3% to at most 6% on that test.
Within up to 5.5% A1c, you are seeing a doubling of mortality from
coronary heart disease, compared with people whose A1c is less than 5%.
By the time you get into the early diabetic range, A1c of 7% or higher,
the increase in the risk of dying from coronary heart disease is 7-fold.
If you go to all-cause mortality, you see the same "staircase effect,"
where every increase within the normal range, an average glucose, is
predicting a measurable increase in the risk of mortality. This is a
very powerful study that draws attention to early dysglycemia, early
escape from normal glucose, being cardiotoxic in ways that were not
previously fully appreciated.
|
 |
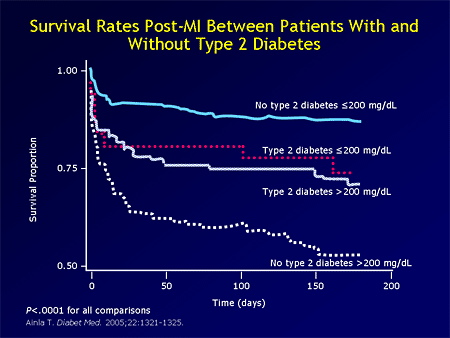
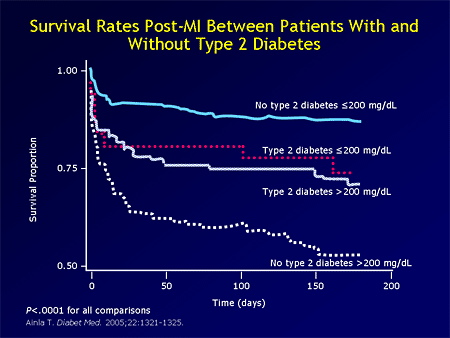
When somebody already has the
diabetes and then suffers a heart attack, we know that the consequences
are disastrous and the prognosis is horrendous. If you do the 200-day
mortality analysis for people with or without diabetes who have suffered
a heart attack, those who do not have type 2 diabetes (or any diabetes
for that matter) and whose in-hospital blood glucose average is lower
than 200 mg/dL have the best survival. Persons who have type 2 diabetes
and whose glucose exceeds 200 mg/dL have at least a 30% decrease in
survival within 200 days.
Look at these data. These are
folks who did not know they had diabetes. The worst category were people
with no known history of diabetes. You get a heart attack, and in the
course of that hospitalization, your glucose runs in the 200 mg/dL range
-- most likely the 5.5 million Americans walking around with diabetes,
but do not know it yet -- those undiagnosed diabetic folks get a heart
attack and get in there. Their glucose is not addressed; because they do
not have the level of diabetes in the entry history and physical (H and
P), nothing is done to address glucose. Look at their survival -- 50%
dead in 200 days. So, there is a gradation of glucotoxic effects
manifesting in the cardiovascular system that precedes the clinical
diagnosis of diabetes, and it then amplifies the risk of dying from
diabetes if an event has occurred.
|
 |
Monodrug vs Combination TherapyMonodrug vs Combination Therapy
Let's switch gears and address
the better part of my talk -- what are we going to do about it, because
so far I have been painting gory pictures of horror stories happening to
our patients. The good part is that we have things to do about it. I
mentioned earlier that most of the pathophysiologic contributors to type
2 diabetes themselves present veritable targets for intervention; so,
you look at the level of myocyte where insulin resistance is most richly
expressed. We do have agents that can reduce insulin resistance and
improve insulin sensitivity. The thiazolidinediones (TZDs), and to some
extent metformin, can improve peripheral insulin sensitivity. If you
look at the excessive glucose production in the liver -- which you
recall is 2- to 3-fold increased in type 2 diabetes compared with
nondiabetic controls -- we have agents (metformin primarily, but all the
TZDs in full dosages) that can be shown to reduce hepatic glucose
production.
The adipocyte issue is most
responsive to TZDs, where the average fall in free fatty acid recorded
can approach 47%, 50% reduction from baseline; that is a major target
for TZD action. There is insulin secretion, of course; we have had
70-plus years of familiarity with using secretagogues to treat type 2
diabetes. They operate on diabetes by stimulating insulin secretion. Of
course, the caveat is that there must be residual beta cells for them to
work. That is why we do not prescribe them routinely to kids with type 1
diabetes, who are bereft of all beta cell function. But, if there are
some cells left, the secretagogues can stimulate them to release some
more insulin, at least for some time.
|
 |
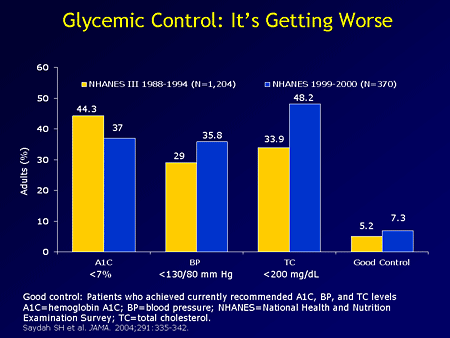
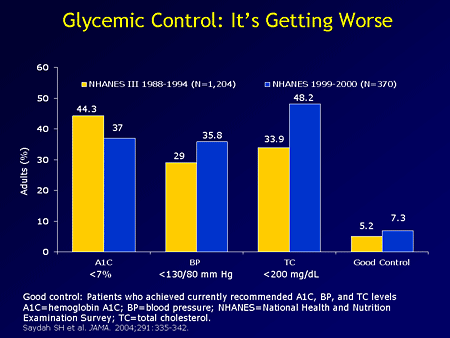
The bad news is that the more
medications we get approved in this therapeutic space, diabetes
management, the worse the national hemoglobin A1c appears to become.
That paradox has not been fully explained to my full understanding. But,
look at the report cards. Clearly, well below 50% of our patients with
diabetes are getting their hemoglobin A1c controlled to the minimally
acceptable target of 7% or lower. The American College of Endocrinology
actually asks for 6.5%, and there are studies that are testing 6% as the
proper goal. So, we are not really accomplishing a lot by way of
control, and that is not an isolated lack of achievement in diabetes,
even in blood pressure management. If you combine diabetic folks who
also have hypertension and high cholesterol, in whom all 3 conditions
are treated to excellent degrees, you are talking about less than 10%.
It has been a challenge.
|
 |
The challenge can be addressed,
in my opinion, by adopting a deliberate policy of combination drug
therapy. One of the weaknesses of chronic disease management is the
patient factor. The patient adherence over prolonged periods of time is
challenging. We can "sneak beneath radar detection," if you will, by
loading on more than 1 chemical to the pill, so that, when patients
think they are taking 1 pill, they actually are taking multiple
medications. That may be one way to address the major problem of lack of
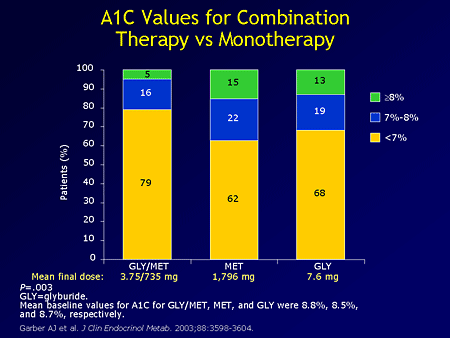
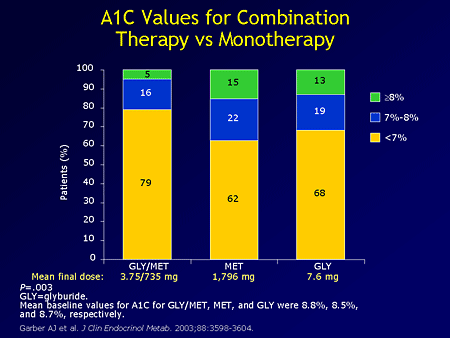
excellence in glucose control. Whenever dual combination therapies have
been pitched against monotherapy, the outcome has always been
predictable. Here you have the glyburide/metformin combination pill
tested against metformin alone in higher dosages (more than twice as
much as was loaded here); or glyburide alone at least twice the dose.
"Half and half" of these drugs will get nearly 80% of your subjects at
the American Diabetes Association (ADA) target of A1c; whereas,
individual drugs titrated to much, much higher milligram dosages failed
to match the combination product.
|
 |
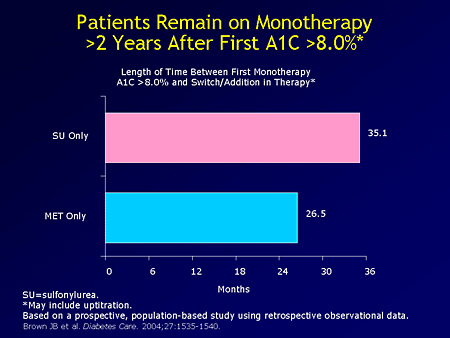
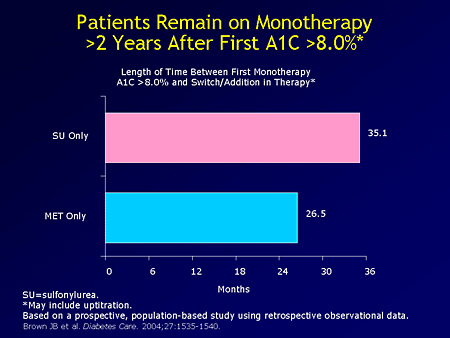
That is an approach that we can
increasingly use; but are we using it? Far from it. This study came out
of the Kaiser Permanente group, a group model health maintenance
organization (HMO), in fact, the granddaddy of all HMOs, where everybody
is insured and has access to all kinds of specialties or interventions.
In that study, Dr. Brown looked at the charts of diabetic patients
whose doctors have registered an A1c of 8% or greater on 1 occasion, and
he looked forward in the chart to when an appropriate action was taken.
An appropriate action being defined as switching to another drug or
adding another diabetes drug onto the one that did not seem to be
working that well, because the patient's A1c was high.
It turned out that it took too
long for any change, any response to high A1c, to be recorded or to be
documented -- more than 1 year, whether patients were initially on Glucophage
(metformin) or on a sulfonylurea. The physicians were waiting too long.
To the extent that Kaiser Permanente doctors are usually well trained,
often multiply board certified, and drawn from a cross-section of the US
demography, they do not mean ill, they are not incompetent -- to that
extent these numbers reflect national habits. I have seen data, not
presented today, where a different set of practitioners was audited and
the numbers were not much better than you see. People are waiting longer
than a year to address high A1c levels.
We need tools also. When we
advocate combination therapy, we need tools that can get patients close
to the goal. The national average A1c is still hovering uncomfortably
closer to 9% and 10%, rather than to the 6.5% that we desire.
|
 |
Effectiveness of Combination Therapies
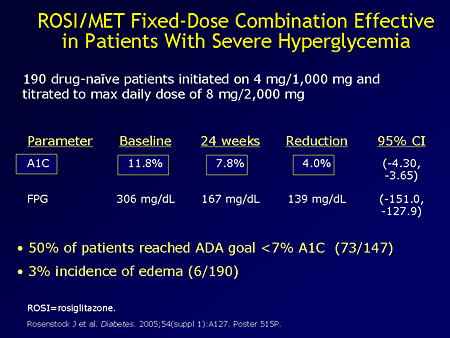
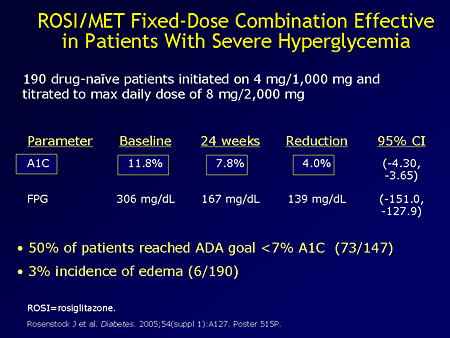
One of the newer products, a drug
that combines rosiglitazone and metformin in a fixed-dose combination
pill, recently has been shown to give us as much as a 4 percentage point
reduction in hemoglobin A1c when used as first-line therapy for
individuals selected for their initially high hemoglobin A1c levels.
Now, I must add that that product (rosiglitazone and metformin, marketed
as Avandamet) has not yet been approved for initial therapy,
but it is approved for later therapy and combination therapy. But this
study is so convincing that I would be surprised if that indication does
not become available soon, because 4 percentage points mean we can
restore many of our patients close to the 7% A1c goal.
|
 |
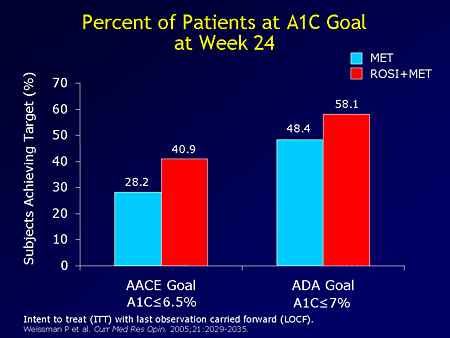
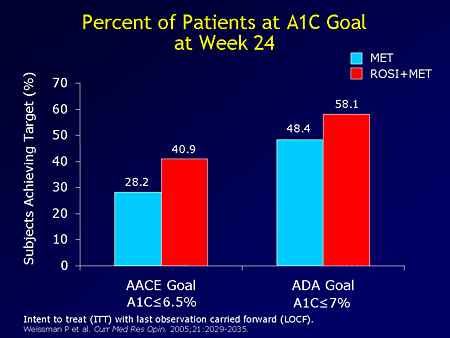
Similar data exist, proving the
point that combination therapy always delivers better quality care than
single agents. Again, I do not want to belabor the point, but, the
percentages reaching both the American Association of Clinical
Endocrinologists (AACE) goal and the ADA goals are higher when the
combination product was administered.
|
 |
Similar studies have used a different thiazolidinedione, a drug called pioglitazone (marketed as Actos).
When combined with metformin, it can give you a nice decrease in
hemoglobin A1c. Metformin is combined with a sulfonylurea drug called
gliclazide (not available in this country but widely used in Britain and
continental Europe). Again, the faster, more rapid action of
sulfonylurea is evident, but the long-term impact is similar between the
2 drugs. Combination therapy works; that is the bottom-line message.
|
 |
In a more recent study,
Rosiglitazone Early vs Sulfonylurea Titration (RESULT), we really have
the point crystallized for us. In this study, individuals were divided
into 2 camps. One-half received titration of a single sulfonylurea drug,
glipizide (Glucotrol), to a maximum dose of up to 40 mg/day.
The other group had half of the maximum dose of sulfonylurea with
rosiglitazone added. Again, you have seen the hemoglobin A1c response to
the combination product being exceedingly greater.
|
 |
Insulin resistance is the bane of
type 2 diabetes, and decreasing that resistance is a target.
Rosiglitazone/sulfonylurea combination group did that, whereas
sulfonylurea alone did not have an impact on the insulin resistance.
|
 |
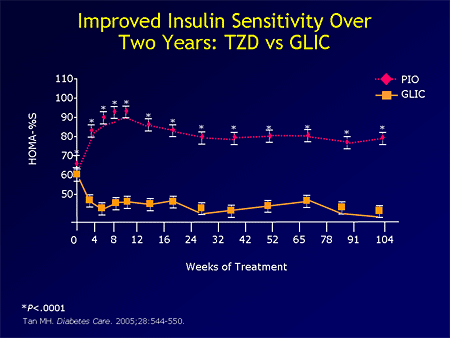
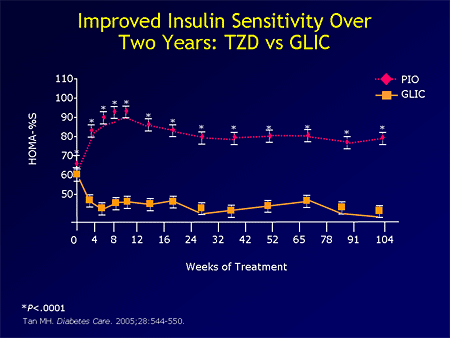
If you look at the same data
using pioglitazone, again, TZDs do improve insulin resistance.
Sulfonylureas do not work on diabetes by altering insulin sensitivity;
they are secretagogues. This is a very well-known point, but from time
to time you may hear presentations that do not fully accord with the
reality. So, no sulfonylurea on the market has an insulin-sensitization
property.
|
 |
Summarizing Combination Therapy
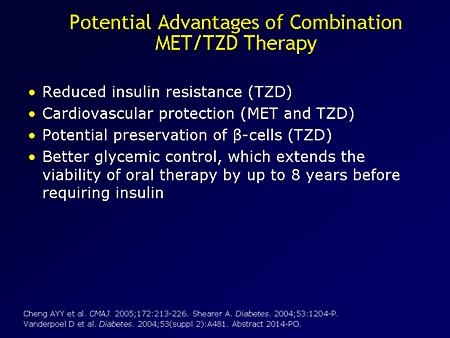
Advantages of TZD-containing preparations have been written about in the literature, but we need studies
|
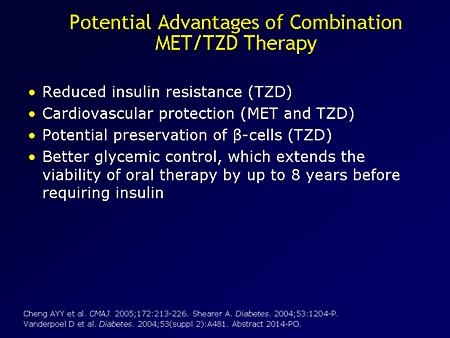 |
The maximization of a single drug
often is not a winning strategy in diabetes management. That has been
repeatedly proven for us. Early recourse to combination therapy is a
smart move. The use of fixed-dose combination strategies might ease
patients into the treatment by optimizing compliance, as compared with
their having to open multiple pill bottles and take them. Aggressive
treatment of diabetes is really the way to go.
|
 |
Cardiovascular Implications of Thiazolidinedione Therapy
I want to show you some quick
clinical trials, one that recently has concluded, others that are
coming. The TZDs, when you look at them, offer so much theoretical
benefit that one often jumps to the conclusion that they ought to be
part and parcel of every diabetes regimen. Well, before we do that, we
need evidence, clinical evidence.
|
 |
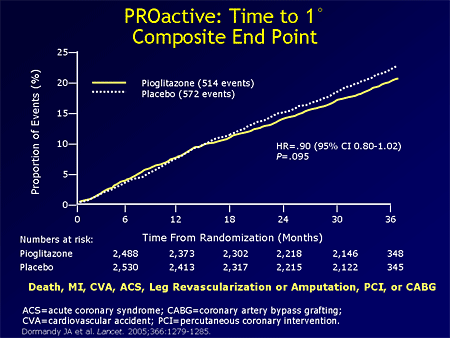
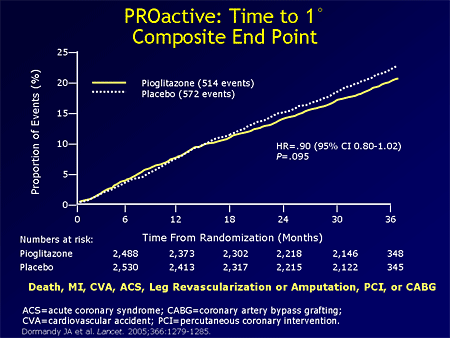
The study here is the PROspective
Pioglitazone Clinical Trial in MacroVascular Events Study (PROactive
study) of patients with type 2 diabetes who have already had
cardiovascular or microvascular events or problems and have multiple
risk factors. They were treated to "standards of care" and then one-half
were given pioglitazone; the other half were not given pioglitazone,
but a matching placebo. They were followed for 36 months. You see a 10%
decrease in the composite primary end points, which included myocardial
infarction (MI), dying from any cause, cardiovascular accident (CVA),
and acute coronary syndrome, among others.
This benefit accruing to the TZD
barely missed statistical significance, and for that reason we say it
was not significant. However, 10% fewer events is clinically meaningful,
1 in 10 fewer events. Why was the primary end point not significant?
The point being made here is that perhaps the group of patients enrolled
for the study were too far gone. Remember, macrovascular complications
begin before clinical diabetes. The presence of diabetes is equivalent
to 1 heart attack. You saw from the data of Haffner and colleagues that
diabetes is a coronary risk equivalent, not a risk factor. Diabetes,
plus events, plus additional risk factors; therefore, it must be a
tertiary prevention study. So, it is even highly impressive that,
despite that late advanced stage, a TZD study is still able to show some
benefit. In fact, when you look at the secondary end points, the
prespecified secondary end points, you get a bigger event reduction and
statistically significant numbers.
|
 |
This is time to acute coronary syndrome.
|
|
This is time to fatal or nonfatal
MI. So, I think that the story continues to look rosy for TZDs. Other
studies in the works have learned from this study and this design. They
are targeting earlier-stage individuals before any heart attack,
sometimes even before diabetes. I will show you some of those studies.
|
 |
Management Issues With the Thiazolidinediones
People gain weight on TZDs. Part
of the weight gain is fluid; the other is actual fat cells being
accumulated. That has discouraged many practitioners from considering
these agents. It also has demoralized some patients from staying on
them.
|
 |
For that reason, a panel was put
together by cardiologists and diabetologists to look into fluid
retention issues with regard to thiazolidinediones. Here is a summary of
the recommendations. I commend the full article to you to look up, but
it is really reassuring. We are quite sanguine with the condition that
less than 1% of congestive heart failure is triggered by TZD
monotherapy. Even for those who are edematous, the edema will not be due
to heart failure in the vast majority of subjects.
However, if cardiac status
deteriorates and crackles begin to be felt in the lung bases, or
shortness of breath occurs, or a cardiologist confirms that there is a
worsening of heart failure, the drug should be stopped. Indeed, no TZD
should be commenced in a patient who is New York Heart Association class
III or IV at baseline.
What happens when somebody gains
some fluid and has demonstrable edema on a TZD? What do we do? Right now
we have been ad-libbing and empirically trying one diuretic or the
other, or a drug holiday.
|
 |
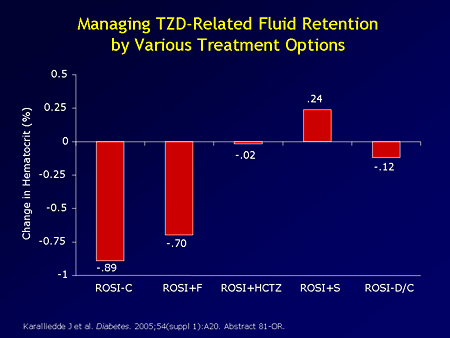
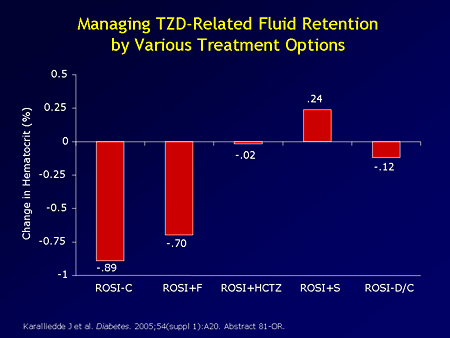
A study is now available that
directs attention to what may work and what may not work. In this study
(using hematocrit dilution as a surrogate for fluid expansion, volume
expansion), 381 patients with type 2 diabetes being treated with
sulfonylurea alone or sulfonylurea and metformin, were then given a TZD,
rosiglitazone. Nearly two-thirds of them developed fluid expansion, as
indicated by a dilution of the hematocrit. They were then randomly
assigned to take furosemide, a loop diuretic; hydrochlorothiazide, a
thiazide diuretic; Aldactone (spironolactone) an
aldosterone-inhibiting potassium-sparing diuretic; or stop the TZD and
see what happens to the fluid retention.
|
 |
This is the first of its kind, of
therapeutic studies, for TZD fluid retention. What became very clear
was that an ordinarily weak diuretic in the grand scheme of things,
spironolactone, proved to be the most potent in preventing fluid
retention on a TZD, followed by thiazide diuretic;. The loop diuretic,
furosemide, was without significant benefit, and compared with
continuing the rosiglitazone, giving furosemide (Lasix) did not
change things much. Stopping the rosiglitazone was moderately effective
in limiting edema; but the best results came when you continued the
rosiglitazone and you gave a 25 mg dose of Aldactone. So, that is something we can use.
|
 |
Safety-wise from the RESULT
study, emergency room visits decreased as did hospitalization rate when
individuals in the TZD, rosiglitazone/sulfonylurea arm were compared
with those whose diabetes treatment was a single drug titrated to the
maximum. The mechanism is not very clear, but it is good news and
reduced cost.
|
|
Studies of Early-Stage Diabetes
In the home stretch, I want to
show you what is in the works. You have seen this graph before. I told
you that, right up to this point, blood tests will not show diabetes in
any of your patients. In this early stage, we begin to see IFG or
prediabetes, and we have had a paucity of studies that have intervened
in that early stage. The PROactive study went beyond late diabetes, for
diabetes plus event, to see if a TZD would change the natural history.
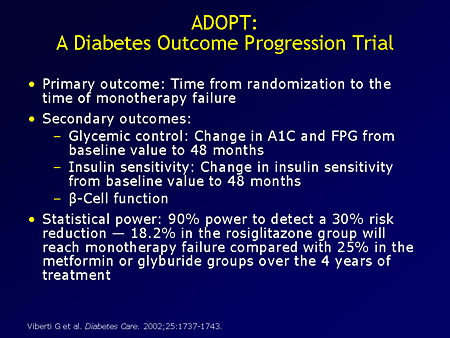
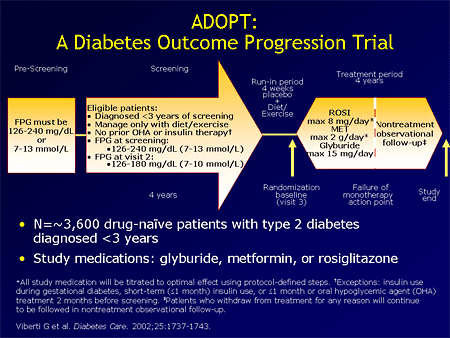
What we have are 2 powerful
studies that are on the horizon of being completed and one about to be
presented. The "A Diabetes Outcome Progression Trial" (ADOPT) trial goes
a little later into early diabetes.
|
 |
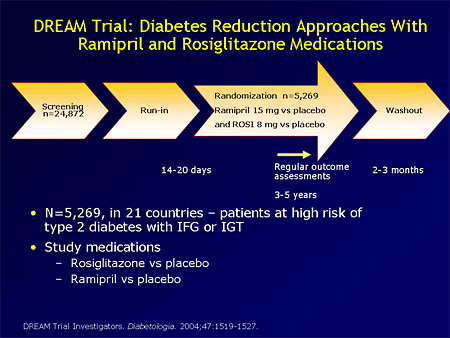
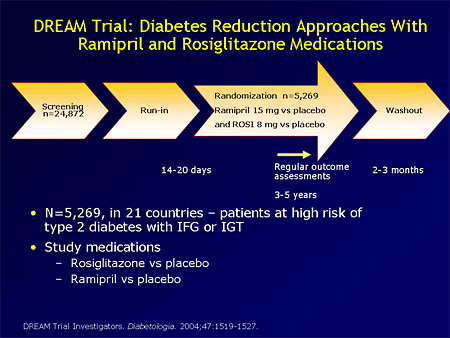
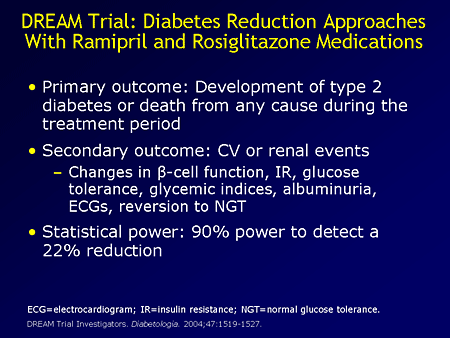
The Diabetes Reduction Approaches
With Ramipril and Rosiglitazone Medications (DREAM) trial is targeting
and has enrolled prediabetics, completely nondiabetic people in the IFG
or IGT range. They are being followed for diabetes as an outcome, as
well as others (long list of coronary, cardiovascular, and total life
outcomes, mortality, etc). These studies are going to be very valuable
in the way we approach diabetes and the way we decide to intervene
early, and what tools we use for early intervention.
In the DREAM trial you have
ramipril, an angiotensin-converting enzyme (ACE) inhibitor, being used
alone or in combination with rosiglitazone, which is also being used
alone or in the combination. Then, you have double placebo; it is a 2 X 2
factorial design. They are being followed after enrollment. They will
stay on protocol a maximum of 5 years and then be washed out.
|
 |
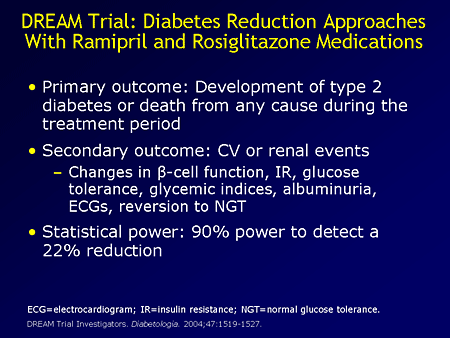
A variety of outcome
measurements, including diabetes, coronary events, stroke, and
macrovascular disease are being tracked. This study is at an advanced
stage of completion, and we will hear results from it before long. It is
powered to the extent of 90% power to detect a 22% reduction in the
intervention arm, so it is well designed.
|
 |
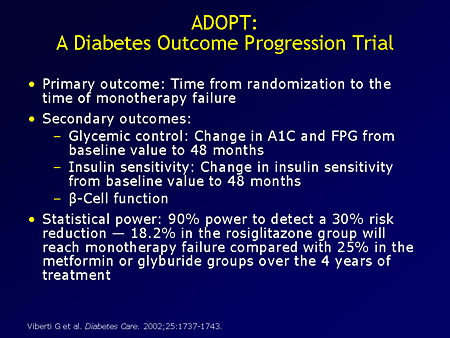
In ADOPT, (this is a very busy
slide), the crux of this trial is that individuals recently developing
diabetes, less than 3 years (on average only 8 months of diabetes
history) would immediately be randomly assigned to take either
glyburide, metformin, or rosiglitazone, representing the 3 most widely
used classes of oral antidiabetic agents.
|
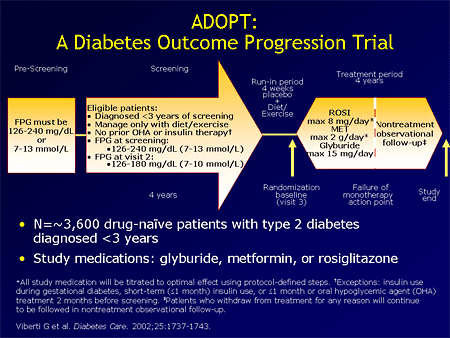 |
They will then be followed for an
end point that consists of a strictly and rigorously defined failure of
monotherapy. We will try to determine which one of these 3 drugs will
carry the most patients the farthest along in a state of good control.
If that result comes to the finishing line and we have the data, we will
be able to share with each other what is the best initial oral agent to
introduce shortly after diagnosis of type 2 diabetes on the basis of
the evidence.
|
 |
|
Finally, I have told you that
there is a diabetes epidemic raging. There is no sign of a crest or a
plateau at all. It is associated with a galaxy of complications that
conveniently can be divided into small-vessel and large-vessel
complications. The large-vessel complications are what kill our
patients, the heart attacks and strokes. They occur even before the
diabetes has become clinical grade, and they are now the target of
antidiabetic interventions, not just the glucose. We have been overly
focused on glucose outcome measures. We are now expanding and demanding
more of our diabetes drugs. What more can we do for our patients with
diabetes besides lowering their glucose? Would we prevent the heart
attack, etc? Studies are on the horizon that will tell us that.
No comments:
Post a Comment